This can lead to post surgical scar tissue. Bands of scar tissue lead to surgical adhesions. In abdominal surgery, for instance, adhesions can cause complications more than 50% of the time.
You feel like you’ve healed up and the external scar looks clean but, little do you know, there may be scar tissue formation under the skin. Months after the surgery, the joint can get stiff leading to problems like frozen shoulder, bowel obstruction, palpable bumps under the skin or chronic pain may begin to develop.
How Does Scar Tissue Differ From Original Tissue?
- Surgical adhesions glue organs and tissues together
- Have less blood supply than original tissue
- Scar tissue is more painful
- Haphazard in its pattern versus organized under a microscope
- Brittle rather than flexible
- Can cause joints to “freeze-up”
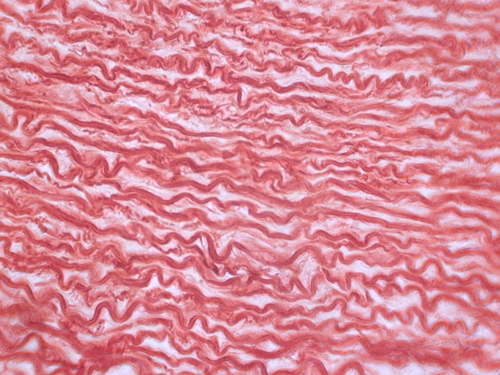
Normal flexible collagen fibers
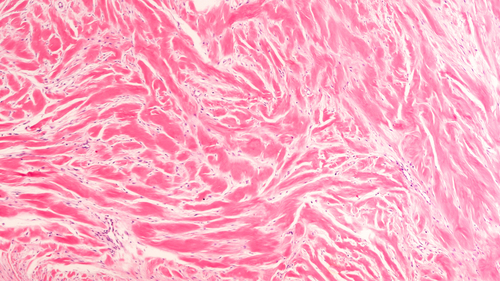
Collagen with scar tissue
How to Decrease Surgical Adhesions with Shockwave Therapy (ESWT)
The medical route can be to cut out scar tissue with a laparoscopic surgery. This can be indicated and help with decreasing bowel obstructions, aiding in fertility or increasing joint mechanics. However, there is a risk of more scar tissue with the laparoscopic surgery.
The Piezowave 2 (the extracorporeal shockwave instrument we use) can penetrate 3cm deep and begin to break up scar tissue on a cellular level [1,2]. When shockwaves are sent into normal tissue it ripples like water when throwing a stone into it. The scar tissue is brittle and it breaks. Your body ends up resorbing the calcium and using it for other body processes while the fibrin is packaged up for disposal.
Then what happens is quite profound. New blood vessels are formed and the tissue re-heals with a stronger, more flexible and organized tissue left [3].
You will have an awareness of the Piezowave 2 doing it’s job. There will be a pulsing feeling and, possibly, a dull ache. Afterwards, people note a feeling of more “freedom” in the area being treated and, often, more mobility in their joints.
Come to our Los Gatos office and have the machine used on your area of concern. We will know the first visit whether we are able to reach your scar tissue or not.
You can reach Dr Adam Fields for in-person (Los Gatos and San Jose, California) or telehealth appointments here.
About Chiropractor Dr Adam Fields
Dr Adam Fields is a practicing chiropractor in the Bay Area in Northern California and helps people daily in his office with many challenges that can be helped by shockwave therapy from tendinopathies, arthritis, cartilage regeneration, post surgical scar tissue, pelvic pain, altered biomechanics and more. He uses Endonasal Cranial Adjusting, the Muncie Technique, Extracorporeal Shockwave Therapy (ESWT), Class IV Laser Therapy, posture correction, lifestyle modification, muscle work, and other techniques to help his patients.

Dr Adam Fields of Los Gatos & San Jose, CA demonstrates ESWT for surgical adhesions post knee surgery
Shockwave Therapy and Post Surgical Scar Tissue Research
- Gerdesmyer L, Wagenpfeil S, Haake M, et al. Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trial. JAMA. 2003; 290:2573-80
- Mittermayr R1, Hartinger J, Antonic V, Meinl A, Pfeifer S, Stojadinovic A, Schaden W, Redl H.Extracorporeal shock wave therapy (ESWT) minimizes ischemic tissue necrosis irrespective of application time and promotes tissue revascularization by stimulating angiogenesis.Ann Surg.
- Ludwig Boltzmann Institute for Experimental and Clinical Traumatology, Vienna, Austria. Rainer.Mittermayr@trauma.lbg.ac.at. Extracorporeal shock wave therapy (ESWT) minimizes ischemic tissue necrosis irrespective of application time and promotes tissue revascularization by stimulating angiogenesis.Ann Surg. 2011 May;253(5):1024-32. doi: 10.1097/SLA.0b013e3182121d6e.